txheem
Cov tshuaj tiv thaiv HPV: zoo tiv thaiv kab mob qog noj ntshav?
In 2015, the annual number of new cases of cancer linked to human papillomaviruses was estimated in France at more than 6. But there are simple ways to protect yourself from this sexually transmitted infection: vaccination and screening.
What is the papillomavirus?
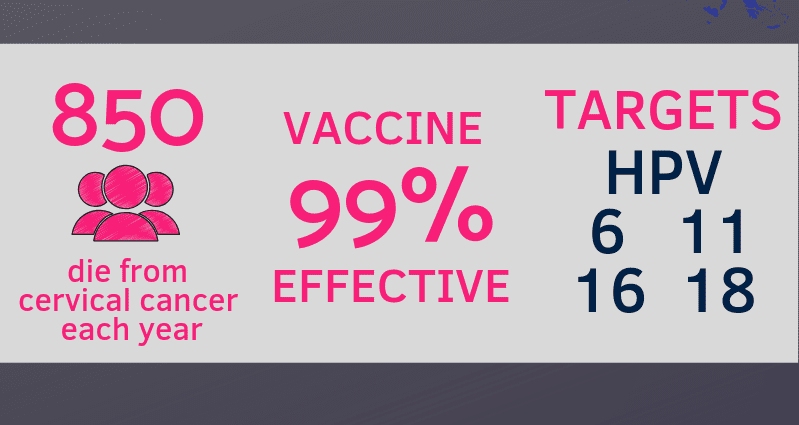
The human papillomavirus, also called HPV, is a sexually transmitted virus, or STI, which can cause genital warts, of varying severity. It is best known for leading to cancers such as that of the cervix for example, which kills nearly 1000 women each year. There are about 150 kinds of papillomavirus. For Delphine Chadoutaud, pharmacist, this virus can also cause “cancers in the rectum or mouth following sexual practices that affect these areas”, but also cancers of the penis, vulva, vagina or throat. .
These cancers take years or even decades to develop asymptomatically. According to the website papillomavirus.fr, “The natural history of cervical cancer begins with an infection caused by a high-risk carcinogenic human papillomavirus. In about 10% of cases, the virus is not spontaneously cleared from the body. The infection becomes persistent and can lead to abnormal cell proliferation and genetic damage. There is then a non-negligible risk of progression to a precancerous lesion and then, in certain cases, to cancer ”.
The papillomavirus vaccine
“Vaccination against human papillomaviruses (HPV) makes it possible to prevent infections by the most frequent papillomaviruses, responsible, in women, for 70 to 90% of cancers of the cervix” describes the health insurance website . However, the vaccine alone does not protect against all cancers or against all precancerous lesions. To limit the risk of cervical cancer, women must be screened regularly by performing a smear of the cervix, from the age of 25. In a study published in October 2020 by the New England Journal of medicine, researchers followed nearly 1 million women aged 10 to 30 over a 10-year period. The results show that among vaccinated women, the rate of cervical cancer was 47 cases per 100 people while it was 000 cases per 94 people for unvaccinated women. It also reveals that women who had been vaccinated against the papillomavirus had an 100% lower risk of contracting cervical cancer than unvaccinated women.
Cov tshuaj tiv thaiv ua haujlwm li cas?
“During vaccination, an antigen is injected which will make it possible to manufacture antibodies in the body” specifies the pharmacist. As the site papillomavirus.fr explains, “These antibodies are present in particular in the vagina, on the surface of the cervix. During sexual intercourse with a partner carrying one of the papillomaviruses covered by the vaccination, the vaccinated person’s antibodies bind to the papillomaviruses and generally prevent them from entering the cells, thus preventing him from being infected ” .
The vaccines available
There are currently three vaccines available against human papillomavirus:
- a bivalent vaccine (which protects against viruses of types 16 and 18): Cervarix®,
- a quadrivalent vaccine (which protects against viruses types 6, 11, 16 and 18): Gardasil®,
- a nonavalent vaccine (which also protects against viruses types 31, 33, 45, 52 and 58): Gardasil 9®.
The vaccines are not interchangeable and any vaccination initiated with one of them must be completed with the same vaccine. The High Council for Public Health (HAS) also recommends that any new vaccination be initiated with the nonavalent Gardasil 9® vaccine.
At what age should you be vaccinated?
For Delphine Chadoutaud, “the vaccine must be done before the start of sexual life to be more effective”. For girls and boys aged 11 to 14, vaccination takes place in two injections spaced 6 to 13 months apart. Between 15 and 19 years old, it is necessary to make three injections: the second injection takes place two months after the first, and the third six months after the first. After 19 years, vaccination is no longer reimbursed by social security. “The vaccination should be discussed with a doctor because the situation is different between a 25-year-old still virgin or a 16-year-old who has already started his sexual life” adds the pharmacist.
Cov kev mob tshwm sim yog dab tsi?
“As with all vaccines, there are side effects. But for this one, the risk-benefit ratio is very favorable ”reassures Delphine Chadoutaud. After the vaccination, it is for example possible to feel numbness in the arm, a bruise, redness where the bite was performed. In rarer cases, some patients suffer from headache, fever or muscle pain. These side effects usually go away within a few days. If they continue, do not hesitate to consult your doctor.
Contraindications
The papillomavirus.fr site warns patients: “side effects should not be confused with contraindications to vaccination which are very rare. Some people cannot be vaccinated for reasons related to their condition. These contraindications (illness, pregnancy for certain vaccines, allergy, etc.) are well known and relate to each vaccine: before prescribing and then before performing a vaccination, the doctor or midwife checks whether or not the person can be vaccinated. at the scheduled time ”.
Leej twg yuav sab laj?
The vaccine against the human papillomavirus can be carried out by a doctor, a midwife, or a nurse on prescription in a free information, screening and diagnosis center (Cegidd), a family planning center and some vaccination centers. public. The vaccine is covered at 65% by social security on presentation of a prescription. Vaccination can also be free in some centers.